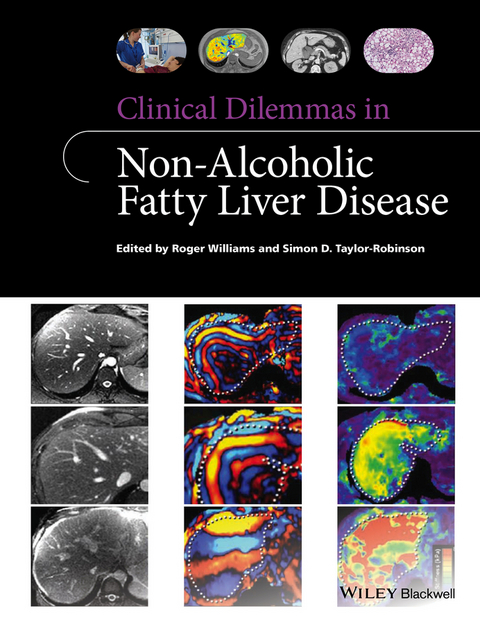
Clinical Dilemmas in Non-Alcoholic Fatty Liver Disease (eBook)
256 Seiten
Wiley-Blackwell (Verlag)
978-1-118-92497-6 (ISBN)
Clinical Dilemmas in Non-Alcoholic Fatty Liver Disease offers hepatologists practical, up-to-date and expert guidance on the most topical dilemmas, difficulties and areas of controversy/difficulty surrounding this ever-increasing area of liver disease they face in daily practice.
Roger Williams and Simon Taylor-Robinson, two of Europe's leading hepatologists, have recruited leading figures from across the world to assist them, resulting in a truly international approach. Each chapter covers a specific area of difficulty, containing clear learning points and providing evidence-based expert guidance on the latest hot topics in clinical management such as:
- Is NAFLD different in absence of Metabolic Syndrome?
- Are the pros outweighed by the cons of obtaining a liver biopsy?
- Is progression to cirrhosis more likely in children with NAFLD?
- What are the dangers as well as the true benefits of bariatric surgery?
- How is it best to use antifibrotic agents in clinical practice?
Clinical Dilemmas in Non-Alcoholic Fatty Liver Disease provides the answers to the questions and challenges that clinicians face every day in this area. It is essential reading for hepatologists of all levels and researchers in hepatology, as well as all those involved in the care of patients with NAFLD, including gastroenterologists, pathologists and specialist hepatology nurses.
Professor Roger Williams CBE, runs the Institute of Hepatology at UCL, and is a twice former president of EASL. He has authored an incredible 2100 journal articles. Despite advancing years, he is still actively involved in clinical research -- 340 articles in the past ten years, and analysis by ISI shows him to be one of the most influential researchers in his field. The award of a CBE for services to medicine recognised his major contribution to the study of liver disorders over 25 years including leading the team who performed the first ever UK liver transplant. He also performed George Best's controversial liver transplant in 2002.
Prof Williams has had many awards, medals, honorary fellowships, and in 2006 was included by HRH The Queen in a celebration at Buckingham Palace to honour those who continue to contribute to public service beyond the age of 65yrs. He was made a Fellow of King's College London in 1992 and an Honorary Fellowship from UCL was conferred on him in 2008, in recognition of his distinguished career and outstanding service to UCL.
Professor Simon Taylor-Robinson joined the Department of Medicine at Imperial College London in 1997, having previously been Senior Registrar in Gastroenterology and Hepatology at Hammersmith Hospital. He was awarded the Sir Francis Avery Jones Gold Medal by the British Society of Gastroenterology in 1999 and the Young Investigator Award of the Liver Section of the European Gastroenterology Association in 1997. He is currently Director of the Imperial Clinical Research Facility at St Mary's Hospital, London.
Professor Roger Williams CBE, runs the Institute of Hepatology at UCL, and is a twice former president of EASL. He has authored an incredible 2100 journal articles. Despite advancing years, he is still actively involved in clinical research -- 340 articles in the past ten years, and analysis by ISI shows him to be one of the most influential researchers in his field. The award of a CBE for services to medicine recognised his major contribution to the study of liver disorders over 25 years including leading the team who performed the first ever UK liver transplant. He also performed George Best's controversial liver transplant in 2002. Prof Williams has had many awards, medals, honorary fellowships, and in 2006 was included by HRH The Queen in a celebration at Buckingham Palace to honour those who continue to contribute to public service beyond the age of 65yrs. He was made a Fellow of King's College London in 1992 and an Honorary Fellowship from UCL was conferred on him in 2008, in recognition of his distinguished career and outstanding service to UCL. Professor Simon Taylor-Robinson joined the Department of Medicine at Imperial College London in 1997, having previously been Senior Registrar in Gastroenterology and Hepatology at Hammersmith Hospital. He was awarded the Sir Francis Avery Jones Gold Medal by the British Society of Gastroenterology in 1999 and the Young Investigator Award of the Liver Section of the European Gastroenterology Association in 1997. He is currently Director of the Imperial Clinical Research Facility at St Mary's Hospital, London.
Title Page 5
Copyright Page 6
Contents 7
List of contributors 9
Preface 11
Part I Nature of the Condition 13
Chapter 1 Non-alcoholic fatty liver disease: Hype or harm? 15
References 17
CHapter 2 NAFLD: A worldwide problem 20
Introduction 20
Prevalence of NAFLD worldwide 21
Disease severity 22
Obesity and metabolic syndrome 23
Genetic predisposition 23
NAFLD as a cofactor 23
Conclusions 24
References 24
Chapter 3 Is insulin resistance the principal cause of NAFLD? 27
Introduction 27
What is meant by insulin resistance? 28
How is insulin resistance measured in vivo in man? 28
Insulin resistance and NAFLD 33
Conclusions 37
References 37
Chapter 4 Paediatric NAFLD: A distinct disease with the propensity for progressive fibrosis 41
Introduction 41
Developmental origins of paediatric NAFLD 42
Paediatric NAFLD: Histological evidence of early progression 42
Paediatric NAFLD: A distinct disease? 42
Ductular reaction, hedgehog signalling and advanced fibrosis 43
What do we know from other types of paediatric chronic liver disease? 44
What are the known risk factors for progression of fibrosis in NAFLD? 44
Conclusion 45
References 45
Chapter 5 Non-alcoholic fatty liver disease (NAFLD) as cause of cryptogenic cirrhosis 48
Introduction 48
Cryptogenic cirrhosis: Definition and characteristics 49
Pathological recognition of NAFLD/NASH in cryptogenic cirrhosis 49
Evidence for NAFLD as the cause of cryptogenic cirrhosis 52
Loss of steatosis in late NAFLD/NASH with cirrhosis 52
Other possible causes of cryptogenic cirrhosis and future directions 52
Summary 53
References 53
Chapter 6 Is NAFLD different in absence of metabolic syndrome? 56
Introduction 56
Metabolically normal NAFLD, Hb, and iron 57
Genetic factors and metabolically normal NAFLD 57
Prognostic implications of metabolically normal NAFLD 58
Does metabolically normal NAFLD require a specific treatment approach? 59
Conclusions 59
References 60
CHapter 7 Occurrence of noncirrhotic HCC in NAFLD 62
The metabolic syndrome, NAFLD, and HCC 63
Pathogenesis linking HCC and NAFLD 64
Conclusions 66
References 67
Part II Factors in Disease Progression 71
Chapter 8 Fibrosis progression: Putative mechanisms and molecular pathways 73
Introduction 73
The concept of liver repair 74
Mechanisms of liver fibrogenesis 74
Key molecular pathways 78
Conclusions and future 81
Acknowledgements 81
References 81
Chapter 9 When is it NAFLD and when is it ALD?: Can the histologic evaluation of a liver biopsy guide the clinical evaluation? 84
Introduction 84
Steatosis 84
Inflammation 87
Hepatocellular injury 87
Fibrosis 88
Other lesions 89
Grading and staging: ALD and NAFLD 91
References 91
Chapter 10 Of men and microbes: Role of the intestinal microbiome in non-alcoholic fatty liver disease 94
Introduction 94
Intestinal microbiome 94
Conclusion 99
References 100
Chapter 11 Can genetic influence in non-alcoholic fatty liver disease be ignored? 103
Introduction 103
What evidence suggests a heritable component to NAFLD? 103
What genetic factors have been identified? 104
Conclusions and clinical relevance 112
References 112
Chapter 12 Is there a mechanistic link between hepatic steatosis and cardiac rather than liver events? 115
Introduction 115
Evidence supporting the association between NAFLD and CVD 116
Mechanistic link between NAFLD and CVD 116
Genetic association between fatty liver and cardiometabolic risk 119
Conclusion 120
References 120
Part III Diagnosis and Scoring 123
Chapter 13 How to best diagnose NAFLD/NASH? 125
Primary or secondary NAFLD? 126
Histological diagnosis 126
Noninvasive diagnostic procedures 128
Recommendations for diagnosis in clinical practice 130
References 132
Chapter 14 The clinical utility of noninvasive blood tests and elastography 136
Introduction 136
Use of noninvasive fibrosis tests in chronic liver diseases 136
Noninvasive diagnosis of NASH 138
Noninvasive fibrosis assessment 139
Conclusions: Future directions 140
References 141
Chapter 15 Are the guidelines—AASLD, IASL, EASL, and BSG—of help in the management of patients with NAFLD? 143
A definition problem 143
To screen or not to screen? 144
The thin line between NAFL and NASH 144
Therapy: An open and evolving question 145
Special population: Pediatric patients 146
Conclusions 146
References 147
Chapter 16 Imaging methods for screening of hepatic steatosis 150
Ultrasound 150
Computed tomography 152
Advantages and limitations of CT for screening 153
Magnetic resonance imaging 153
Qualitative estimation of hepatic fat on MRI 154
Quantitative estimation of hepatic fat on MRI 156
MRS 157
References 160
Chapter 17 Are the advantages of obtaining a liver biopsy outweighed by the disadvantages? 164
Introduction 164
Diagnosis and assessment of disease severity 164
Technical and logistical matters 168
Conclusions 169
References 170
Chapter 18 Screening for NAFLD in high-risk populations 173
Introduction 173
Nature of NAFLD: Relevance to screening 173
Current opinion and guidelines 173
The high-risk population 174
Potential screening tests 175
A practical approach to NAFLD screening 178
Summary 180
References 180
Part IV Value of Treatment Measures 183
Chapter 19 Defining the role of metabolic physician 185
Diagnosis and assessment of the obese patient 187
Medical management of obesity 189
Management of bariatric surgical patients 190
Conclusions 191
References 191
Chapter 20 Should physicians be prescribing or patients self-medicating with orlistat, vitamin E, vitamin D, insulin sensitizers, pentoxifylline, or coffee? 194
Introduction 194
Coffee consumption 194
Orlistat 195
Pentoxifylline 196
Vitamin E 196
Insulin sensitizers 197
Vitamin D 198
Conclusion 198
References 198
Chapter 21 Effects of treatment of NAFLD on the metabolic syndrome 201
Introduction 201
Effect of insulin-sensitizing antidiabetic treatments on NAFLD and the MetS (Table 8.1) 202
Conclusions 205
References 205
Chapter 22 What are the dangers as well as the true benefits of bariatric surgery? 208
Introduction 208
Development of bariatric surgical procedures 209
What are the risks of bariatric surgery? 212
Benefits of bariatric surgery 213
Conclusion 214
References 214
Chapter 23 Liver transplantation: What can it offer? 215
Current results of liver transplantation for NASH 216
Frequency of NAFLD recurrence and of metabolic syndrome after transplantation and clinical significance 216
Impact of obesity on long-term outcome after liver transplantation for non-NASH indications 218
Conclusion 219
Acknowledgement 219
References 219
Part V What Does the Future Hold? 221
Chapter 24 Molecular antagonists, leptin or other hormones in supplementing environmental factors? 223
Introduction 223
Strategies to promote ‘healthier’ adipose tissue function 223
Beyond diabetes and insulin signalling 224
Lipid and dietary modification 225
Hepatic oxidative stress 226
Conclusion 226
Acknowledgement 227
References 227
Chapter 25 What is the role of antifibrotic therapies in the current and future management of NAFLD? 230
Antifibrotic targets in NAFLD 230
Challenges of clinical trial design in NAFLD 231
What have we learnt from NAFLD antifibrotic trials to date? 232
What are the most promising emerging antifibrotic therapies in NAFLD? 232
Other emerging therapies 235
Conclusions 235
Acknowledgement 235
References 235
Chapter 26 Developmental programming of non-alcoholic fatty liver disease 238
Human studies 239
Animal models 239
Cellular and subcellular mechanisms 239
Nervous system 240
Epigenetic mechanism 240
Immune mechanism 240
Gut microbiota 240
Conclusions 242
References 242
Index 244
Supplemental Images 252
EULA 264
| Erscheint lt. Verlag | 17.2.2016 |
|---|---|
| Reihe/Serie | Clinical Dilemmas | Clinical Dilemmas (UK) |
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Allgemeines / Lexika |
| Medizinische Fachgebiete ► Innere Medizin ► Gastroenterologie | |
| Medizinische Fachgebiete ► Innere Medizin ► Hepatologie | |
| Schlagworte | Fatty Liver Disease • Gastroenterologie • Gastroenterologie u. Hepatologie • Gastroenterology & Hepatology • Hepatologie • hepatology • liver disease • liver inflammation • Medical Science • Medizin • Metabolic disease • NAFLD • Nash • Non-alcoholic fatty liver disease • Non-alcoholic steatohepatitis • Stoffwechselkrankheit • Stoffwechselkrankheiten |
| ISBN-10 | 1-118-92497-5 / 1118924975 |
| ISBN-13 | 978-1-118-92497-6 / 9781118924976 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: PDF (Portable Document Format)
Mit einem festen Seitenlayout eignet sich die PDF besonders für Fachbücher mit Spalten, Tabellen und Abbildungen. Eine PDF kann auf fast allen Geräten angezeigt werden, ist aber für kleine Displays (Smartphone, eReader) nur eingeschränkt geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich